Diabetic Eye Disease Treatment in Bagdogra: As many as 50 million people are suffering from type-2 diabetes in India. However, medical experts feel that timely detection and right management can go a long way in helping patients lead a normal life. Diabetes is a chronic medical condition, that is, it can be curbed at the initial level by introducing lifestyle changes and controlled after its incidence through medicines in early stages and administration of external insulin in advanced stages. But it would not be wrong to say that it cannot be cured completely and lasts a lifetime.
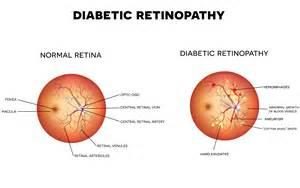
A diabetic eye disease is a group of eye conditions that can affect people with diabetes. If you have diabetes, your blood glucose, or blood sugar, levels are too high. Over time, this can damage your eyes. The most common problem is diabetic retinopathy. It is a leading cause of blindness for people with diabetes.
However, early detection and treatment at our Diabetic Eye Disease Treatment Centre in Bagdogra can reduce the risk of blindness by 95 percent. Because diabetic retinopathy often lacks early symptoms, people with diabetes should get a comprehensive dilated eye exam at least once a year. People with diabetic retinopathy may need eye exams more frequently which can be availed in our eye hospital at low cost.
Diabetic eye disease also includes cataract and glaucoma:
All forms of diabetic eye disease have the potential to cause severe vision loss and blindness.
In most cases, early stages present no symptoms. You may not notice it at first. Symptoms can include
Vision lost to diabetic retinopathy is sometimes irreversible. However, early detection and treatment can reduce the risk of blindness by 95 percent. Because diabetic retinopathy often lacks early symptoms, people with diabetes should get a comprehensive dilated eye exam at least once a year. People with diabetic retinopathy may need eye exams more frequently. Women with diabetes who become pregnant should have a comprehensive dilated eye exam as soon as possible. Additional exams during pregnancy may be needed.
Treatment for diabetic retinopathy is often very effective in preventing, delaying, or reducing vision loss. But it is not a cure for the disease. People who have been treated for diabetic retinopathy need to be monitored frequently by an eye doctor to check for new changes in their eyes. Many people with diabetic retinopathy need to be treated more than once as the condition gets worse. Also, controlling your blood sugar levels is always important. This is true even if you have been treated for diabetic retinopathy and your eyes are better. In fact, good blood sugar control is especially important in this case so that you can help keep your retinopathy from getting worse
Laser treatment (photocoagulation) is usually very effective at preventing vision loss if it is done before the retina has been severely damaged. Surgical removal of the vitreous gel (vitrectomy) may also help improve vision if the retina has not been severely damaged. Because symptoms may not develop until the disease becomes severe, early detection through regular screening is important. The earlier retinopathy is detected, the easier it is to treat and the more likely vision will be preserved. You may not need treatment for diabetic retinopathy unless it has affected the center (macula) of the retina or, in rare cases, if your side (peripheral) vision has been severely damaged.But you do need to have your vision checked every year.
Fluorescein angiography is an established technique for examining the circulation of the human retina. In particular it enables the progression of diabetic retinopathy to be monitored and provides valuable information on the presence, or otherwise, of vascular lesions such as oedema (leakage) and ischaemia (occlusion of the capillaries). The method outlined below allows such changes to identified. A fluorescein angiogram is obtained by photographing the fluorescence emitted from the vessels of the retina after intravenous injection of 5ml of 10% sodium fluorescein. The retina is illuminated with a flash of blue light (490nm) and the yellow-green fluorescent light (530nm) is captured on photographic film by inserting an appropriate filter in the reflected light”s path.
The fluorescein dye takes around 10 seconds to reach the patient”s retinal circulation after injection into the patient”s arm. Photography commences immediately after the fluorescein appears in the choroidal circulation, at a rate of around one per second for the first 15 to 20 seconds. Further frames are taken less frequently up to around 5 minutes
Anti-VEGF factors have revolutionised the treatment of diabetic retinopathy. They when given intra-vitreally, cause decrease in retinal swelling and also reduce the stimuli for new abnormal vessels to grow. Also repetitions of such injections have caused improved vision in cases with severe edema, however laser photocoagulation needs to be done as definitive treatment.
Bevacizumab and ranizibumab are two common such products which have been used extensively, ranizubimab is smaller molecule with more specificity.
OCT or optical coherence tomography has revolutionised the management of retinal problems. They are like living autopsy, giving details of layers of retina and d measurements for retinal thickness. This helps in initial diagnosis, as well as follow up of cases, and is non- invasive technique. Patients of diabetic retinopathy do need OCT to regular intervals with comparision scans to evaluate the effect of treatment and progression of disease.