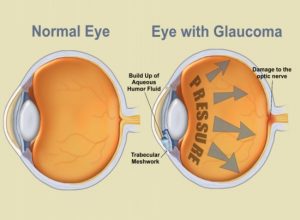
Glaucoma Treatment in Bagdogra: Glaucoma is one of the leading causes of irreversible blindness in the world, especially for older people. However visual loss is preventable or stabilized with early diagnosis and treatment. Glaucoma is a condition of the eye where the optic nerve is damaged. The optic nerve carries images to the brain, which are then perceived as vision. Minute nerve fibres from various parts of the retina join to form the optic nerve. Glaucoma results when the pressure within the eye is high enough to be detrimental to the normal functioning of these nerve fibres, some of which stop functioning. Non-functional nerve fibers result in a loss of retinal function in the area from where they originate, leading to defects in the field of vision. Vision Eye Care’s affordable Glaucoma Treatment in Bagdogra can help you prevent the visual loss.
The disease is called the sneak thief of sight because it is painless, symptom-less and irreversible. Therefore, the person with glaucoma is usually unaware of it until much loss of vision has occurred. In fact, half of those suffering damage from glaucoma do not know it. Only one type of glaucoma called angle-closure glaucoma is associated with a red, painful eye with blurred vision and even possibly nausea and vomiting. This is due to very high pressures resulting FROM a block in the drainage system of the eye. Most patients at risk for this type of glaucoma have structural differences in their eye which could be identified prior to an attack and preventative treatment could be performed.
Currently, damage from glaucoma cannot be reversed and if the entire nerve is damaged, blindness results. Early detection and regular treatment are the keys to preventing optic nerve damage and blindness from glaucoma. Contact us now to get the best Glaucoma Treatment in Bagdogra from Vision Eye Care, a renowned Eye Care Hospital
Majority of Glaucoma’s can occur and progress without obvious symptoms or signs. Open-angle glaucoma is the most common, and symptoms are slow to develop. As this types of glaucoma progresses, you may notice that your side, or peripheral, vision is failing, causing you to miss objects out of the side and corner of your eye.
If you are suddenly experiencing the following symptoms, you may have angle-closure glaucoma and should seek immediate treatment (Angle Closure accounts for only 1/3rd of all glaucoma’s) and that too the patient should not wait for these symptoms to appear, routine check-up can pick angle closure glaucoma much early:
Glaucoma is basically a nerve disorder characterized by progressive loss of cells. Increased/high intraocular pressure is one feature of this disease and this does not necessarily mean that people with low intraocular pressure cannot have glaucoma. Awareness of the different causes and risk factors for glaucoma may help you identify the condition early on, as timely diagnosis of glaucoma is vital to preventing vision loss.
Everyone should be concerned about glaucoma and its effects. It is important for each of us, from infants to senior citizens, to have our eyes checked regularly, because early detection and treatment of glaucoma are the only ways to prevent vision impairment and blindness. There are a few conditions related to this disease that tend to put some people at greater risk. This may apply to you if:
There are also several medical conditions that increase a person’s risk of glaucoma, including:
There are many different types of glaucoma. The glaucoma’s usually affect both eyes, but the disease can progress more rapidly in one eye than in the other. Involvement of just one eye occurs only when the glaucoma is brought on by factors such as a prior injury, inflammation, or the use of steroids in that eye. The different types of glaucoma are
It is the most common type of glaucoma; damages vision gradually and painlessly. The pressure is rarely high enough to be symptomatic.
An acute attack of glaucoma caused by sudden blockage of the drainage channels leads to a sharp rise in pressure within the eye causing blurred vision, severe eye pain, nausea and vomiting, headache, rainbow haloes around lights, pain around your eyes after watching TV or after leaving a dark theatre and red eyes.
An acute attack requires the immediate attention of an eye doctor.
Developmental glaucoma refers to those glaucomas associated with developmental anomalies that present at birth, including primary congenital glaucoma and glaucoma associated with other developmental anomalies, either ocular or systemic.
An eye doctor (ophthalmologist) can usually detect those individuals who are at risk for glaucoma (because of, for example, a narrow filtering angle or increased intraocular pressure) before nerve damage occurs. The doctor also can diagnose patients who already have glaucoma by observing their nerve damage or visual field loss.
The following tests, all of which are painless, may be part of this evaluation:
The main treatment for chronic glaucoma aims at reducing the pressure in your eye. Damage already caused by glaucoma cannot be reversed. Eye drops, tablets, laser and surgical operations are used to prevent or slow further damage from occurring. With any type of glaucoma periodic examinations are very important to prevent loss of vision. Because glaucoma can irreversibly worsen without your being aware of it, your treatment may need to be changed from time to time during the periodic examination.
Medical treatment
When taken regularly and continuously as prescribed, they control the eye pressure either by slowing the formation of aqueous fluid within the eye or by increasing the flow at the drainage area.
These are sometimes combined with the eye drops to decrease higher levels of eye pressure. They are occasionally known to cause tingling of fingers and toes, bowel irregularities, and in the very long term, kidney stones.
Why a drug causes side effects in some persons and not others is not fully understood.
Lasers of different typesare usually used in one of three ways:
In open-angle glaucoma the draining area itself is enlarged to control eye pressure.
In angle-closure glaucoma the laser creates a hole in the iris to open up and improve the flow of aqueous fluid to the drain.
In painful late-stage glaucoma medication or surgery do not control the pressure. The laser closes some aqueous fluid-producing areas in the eye and lowers the eye pressure.
A new drainage channel is created for the aqueous fluid to leave the eye. Sometimes a tube drains the fluid in very resistant cases.
Surgery is recommended when your doctor feels that it is safer to operate than to allow optic nerve damage to continue.
The best treatment for you should be decided after a thorough examination and discussion with your Glaucoma specialist.
Key points to remember to minimize the risk of glaucoma